Antibiotic resistance Pregled
UNIVERZITET “BIJELJINA”
FAKULTET ZDRAVSTVENIH STUDIJA
PREDMET: ENGLESKI JEZIK
TEMA: ANTIBIOTIC RESISTANCE
PREDMETNI PROFESOR:
STUDENT:
Jovana Vujić
Nedeljko Čavić
BROJ INDEKSA:
169/19
Bijeljina, 2020. god.
1
TABLE OF CONTENTS
1. Introduction....................................................................................................2
2. Origin of antibiotic resistance........................................................................3
3. Development of antibiotic resistance.............................................................5
4. Classification of antibiotics............................................................................7

3
2. Origin of antibiotic resistance
Antibiotic resistance was reported to occur when a drug loses its ability to inhibit
bacterial growth effectively. Bacteria become ‘resistant’ and continue to
multiply in the presence of therapeutic levels of the antibiotics. Bacteria, when
replicated even in the presence of the antibiotics, are called resistant bacteria.
Antibiotics are usually effective against them, but when the microbes become
less sensitive or resistant, it requires a higher than the normal concentration of
the same drug to have an effect. The emergence of antimicrobial resistance was
observed shortly after the introduction of new antimicrobial compounds.
Antibiotic resistance can occur as a natural selection process where nature
empowers all bacteria with some degree of low-level resistance. For example,
one study confirmed that sulfamethoxazole and trimethoprim (TMP-SMZ),
ampicillin and tetracycline that were commonly used in yesteryears, but now
have no longer role in treating non-cholera diarrhea disease in Thailand. At the
same time, another study conducted in Bangladesh showed the effectiveness of
the same drugs in treating them effectively. In fact, resistance was documented
even before the beginning of the usage of the antibiotics in fighting the infection.
Non-judicial use of antibiotic is responsible for making microbes resistant.
Since the introduction of sulfonamides in 1937, the development of specific
mechanisms of resistance had provoked their therapeutic use.
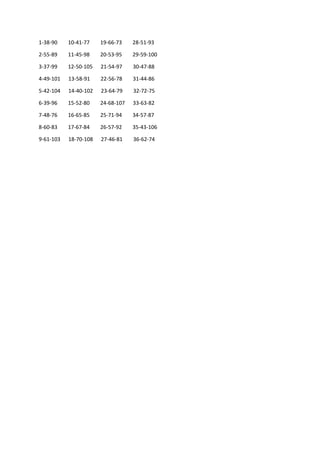
Figure 1 -
Graphical representation of onset of antibiotic resistance versus time to get antibiotic resistance
4
However, sulfonamide resistance was reported in the 1930s, which reveals the
same mechanism of resistance that still operates even now, more than 80 years
later. Within six years of the production of the aminoglycosides,
aminoglycoside-resistant strains of Staphylococcus aureus were developed.
Introduced in 1961, Methicillin was the first of the semisynthetic penicillinase-
resistant penicillin to target strains of penicillinase-producing Staphylococcus
aureus. However, resistance to methicillin was reported soon after its initiation.
Further, although fluoroquinolones were introduced for the treatment of Gram-
negative bacterial diseases in the 1980s, fluoroquinolones resistance later
revealed that these drugs were also used to treat Gram-positive infections.
Quinolone resistance emerged as a stepwise attainment of chromosomal
mutations, particularly among the methicillin-resistant strains. Most recently,
the clinical isolates of Vancomycin-resistant Staphylococcus aureus (VRSA)
were found in 2002, after 44 years of Vancomycin introduction to the market.
Antibiotics used in agriculture are often the same or similar to antibiotic
compounds used clinically, this over-usage could also invite drug resistance.
The food chain can be considered the main route of transmission of antibiotic-
resistant bacteria between animal and human populations. In some developed
countries, animals receive antibiotics in their food, water, or parenterally which
may be responsible for carrying microbe resistance to that specific antibiotic.
For example, the use of antibiotics in cattle feed as growth promoters increase
antibiotic resistance.
Želiš da pročitaš svih 16 strana?
Prijavi se i preuzmi ceo dokument.
Slični dokumenti

Ovaj materijal je namenjen za učenje i pripremu, ne za predaju.